As we all know, tumor tissue is not only composed of cancer cells, it also contains other types of cells. These other cell types can affect tumor behavior and have a profound impact on whether the tumor will respond to therapy, including immunity therapy etc. Fibroblasts are distributed throughout the body. In the colon, they are a part of the body’s contraction system that is critical to digestion. Researchers now know that the presence of fibroblasts in tumors affects its behavior, especially the tumor’s response to immune checkpoint blockers.These blockers can relieve the suppression of the immune system and promote its attack on cancer cells. So far, an unresolved question in this research field is what causes these fibroblast-filled tumors to continue to progress?
Recently, in a research report published in the international journal Developmental Cell, scientists from the Sanford Burnham Prebys Institute for Medical Discovery and other institutions discovered the reason why a type of colon cancer does not respond to immunotherapy. By targeting these factors that interfere with tumor treatment, it may be expected to help develop new methods that make cancer therapies more effective.
In the article, the researchers analyzed CMS4 colorectal cancer and proposed that cancer-related fibroblasts interfere with tumor treatment. CMS4 is one of the most malignant and difficult-to-treat colorectal cancers, and affects the health of nearly one-third of colorectal cancer patients. The researcher aims to determine how these cancer-related cells acquire the properties that promote their support for the carcinogenesis of nearby cells. This research consists of two important components. First, the researchers demonstrated in a obvious way how these cancer-related fibroblasts acquired the characteristics they possess. Second, the scientists confirmed that the findings of the study also apply to patients, and began to reveal how these findings are applied in the clinic.
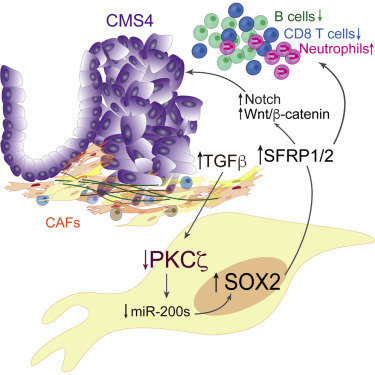
In previous studies, researchers developed a mouse model that mimics CMS4 colorectal cancer. Like this type of colorectal cancer patients, researchers also found high concentrations of cancer related fibroblasts in the tumors of these mice The researchers used mouse models, cultured cells and organoids to study the relationship between cancer cells and cancer-related fibroblasts. They found that cancer cells can send signals to change the characteristics of fibroblasts. Appearing makes the tumor more aggressive and more invisible to the immune system. At the molecular level, it appears to reduce the level of PKCz protein, thereby increasing the level of SOX2 protein in fibroblasts. And then, SOX2 directly binds to the Sfrp1 / 2 promoter, causing the expression of Sfrp1 / 2. Interestingly, the inactivation of Sox2 or Sfrp1/2 in Cancer associated fibroblasts weakens the migration and invasion induction of colon cancer cells, as well as their tumorigenicity in vivo. Therefore, these changes seem to make fibroblasts friendly to promote tumor growth.
The researchers then used animal models to detect the behavior of the changed cells in the laboratory. They used single-cell RNA sequencing technology to confirm that the results observed in the laboratory were consistent with those observed in patient samples; the researchers said that they currently Understanding the communication mechanism between cancer cells and fibroblasts, they believe that the communication between the two allows fibroblasts to protect tumor cells from the human immune system in a unique way.
Subsequent research focuses on finding drugs or methods that can target fibroblasts that deprive the tumor of the protective environment. These drugs can be used in combination with immunotherapy to reduce the defense of fibroblasts and promote the function of immune cells activated by checkpoint blocking drugs. The results of this study may be applied to other cancer types, especially pancreatic cancer. Pancreatic cancer contains a large number of fibroblasts, which seems to make tumors resistant to immune therapy.
