Streptococcus pneumoniae is a class of Gram-positive pathogenic bacteria that was first isolated in 1881. The chemical composition of the mucus layer on the surface of Streptococcus pneumoniae is a polysaccharide capsule, which is the main pathogenic substance of Streptococcus pneumoniae and has antigenicity. According to its structural specificity, Streptococcus pneumoniae can be divided into more than 90 serotypes, of which 10 are the most common serotypes (1, 4, 5, 6B, 7F, 9V, 14, 18C, 19F, 23F). They are responsible for 62% of associated invasive disease worldwide. Inoculation of polyvalent Streptococcus pneumoniae capsular polysaccharide vaccine is an effective way to prevent Streptococcus pneumoniae-related diseases, and the application of this type of vaccine has greatly reduced the incidence of pneumonia. Since Jiamo polysaccharide is a T cell-independent antigen, it cannot produce high-affinity antibodies and immune memory, so it is not suitable for infants and young children. Combining the capsular polysaccharide of Streptococcus pneumoniae with various protein substances can improve the immunogenicity of pneumonia vaccine, stimulate the production of memory antibodies and expand its application range. Pneumonia conjugate vaccine) has come out one after another, and other pneumonia conjugate vaccines are in the clinical development stage. This article reviews the research progress of pneumonia conjugate vaccine development, preparation methods and immunogenicity influencing factors.
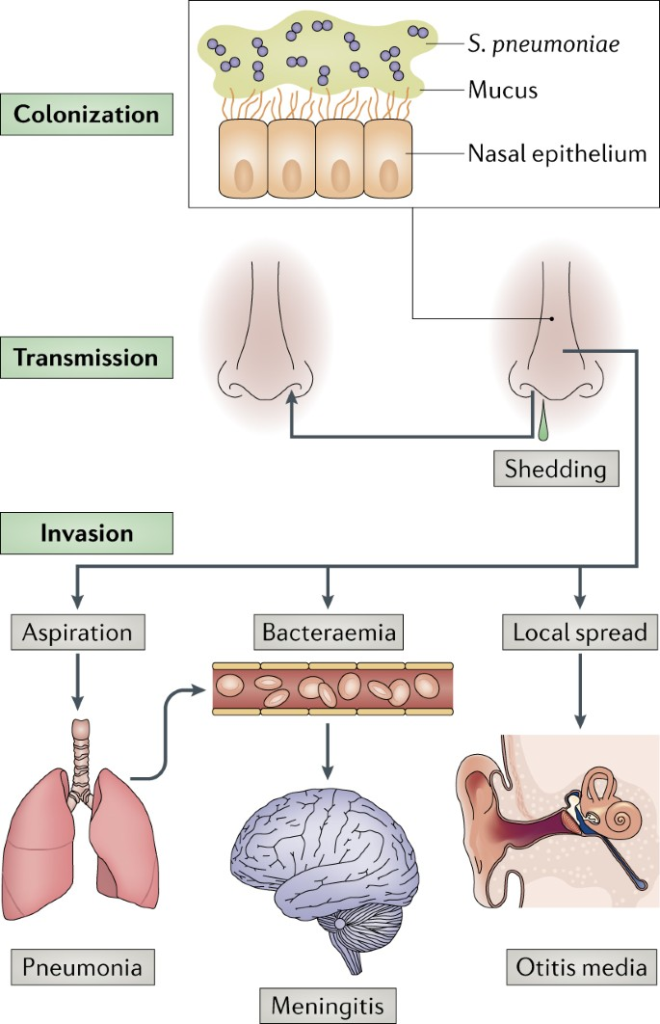
Figure 1. Streptococcus pneumoniae: transmission, colonization and invasion.
Streptococcus pneumoniae Vaccine Development
Streptococcus pneumoniae Capsular Polysaccharide Vaccine
Bacterial capsular polysaccharide is an immunogenic non-protein substance in the human body. Antibodies produced by the body against capsular polysaccharide can effectively prevent the infection of Streptococcus pneumoniae. In 1945, the tetravalent capsular polysaccharide (serotype 1, 2, 5 and 7) have immune effect, and then multivalent Streptococcus pneumoniae polysaccharide vaccines have come out one after another. In 1946, the United States approved for the first time 2 Streptococcus pneumoniae vaccines containing 6 serotypes; in 1977, a 14-valent Streptococcus pneumoniae capsular polysaccharide vaccine (including serotypes 1, 3, 4, 6A, 6B, 7F , 8, 9N, 12F, 14, 18, 19F, 20, 23F)) was successfully registered; in 1983, 23-valent Streptococcus pneumoniae capsular polysaccharide vaccine (including serotypes 1, 2, 3, 4, 5, 6B, 7F, 8, 9N, 9V, 10A, 11A, 12F, 14, 15B, 17F, 18C, 19F, 19A, 20, 22F, 23F and 33F) approved for marketing, the vaccine serotype can cover 90% of drug-resistant strains in the United States and 85%- 90% of the prevalent strains. The 23-valent Streptococcus pneumoniae capsular polysaccharide vaccine is the most serotype-containing product on the market so far. After adults are immunized, the specific antibodies are significantly improved, but nearly 20% of the elderly have a low immune response to it and cannot induce high-affinity antibodies. And immune memory, also not suitable for infants and young children under 2 years old.
Polyvalent Pneumonia Conjugate Vaccine
The covalent coupling between Streptococcus pneumoniae capsular polysaccharide and protein can rapidly stimulate immune response and induce immune memory antibody, which can be used in infants and young children, making up for the deficiency of capsular polysaccharide vaccine. In 2000, Prevenar developed by Pfizer became the first 7-valent pneumonia conjugate vaccine on the market, consisting of 7 serotypes of capsular polysaccharides (serotypes 4, 6B, 9V, 14, 18C, 19F, 23F) and diphtheria toxoid The mutant CRM197 is covalently combined, and the WHO evaluation proves that the vaccine has high safety. With the promotion of immunization with this product, the incidence of pneumococcal disease has dropped significantly, while non-vaccine serotype pneumococcal infection has increased accordingly. To address the above problems and improve the immune performance of pneumonia conjugate vaccines, Synflorix 10-valent pneumonia conjugate vaccines (serotypes 1, 4, 5, 6B, 7F, 9V, 14, 18C, 19F, 23F) of GlaxoSmithKline and Prevenar13 of Pfizer (serotypes 1, 3, 4, 5, 6A, 6B, 7F, 9V, 14, 18C, 19A, 19F, 23F) has been approved for marketing. Both of these two vaccines can stimulate a strong immune response, and have high safety and tolerance, and both can induce an immune response in infants, further expanding the scope of application of the pneumonia conjugate vaccine. The serotype coverage rates of Synflorix10 and Prevenar13 vaccines in immunized areas were 70%-84% and 74%-88%, respectively.
Research Progress of Polyvalent Pneumonia Conjugate Vaccine
The 15-valent pneumonia conjugate vaccine V114 developed by Merck added 22F and 33F serotypes on the basis of Prevenar13. The phase II clinical trial results of this vaccine showed that after healthy infants were immunized with V114 and 13-valent conjugate vaccines, the increased 22F in V114 and 33F serotypes reached 98% and 87% of the immune criteria, respectively. In February 2019, Pfizer developed a 20-valent pneumococcal conjugate vaccine, which contains 8, 10A, 11A, 12F, 15B/C, 22F and 33F 7 kinds of serotypes, in addition to the serotypes included in the marketed 13-valent pneumococcal conjugate vaccine, expanding the scope of immunity of Streptococcus pneumoniae vaccine.
Preparation Method of Pneumonia Conjugate Vaccine
Direct Combination Method
The direct binding method uses the inherent functional groups on the surface of the Streptococcus pneumoniae capsular polysaccharide to covalently couple with the functional groups on the surface of the protein carrier. The abundant functional groups on the surface of the polysaccharide facilitate direct binding to the protein. The amine reduction method used in Pfizer’s 13-valent pneumonia conjugate vaccine is a typical direct conjugation method.
Indirect Combination Method
Indirect Binding Method
The indirect binding method uses a linking agent to covalently bind the Streptococcus pneumoniae capsular polysaccharide and the carrier protein. This method can reduce the spatial shielding effect and thus affect the immunogenicity of the conjugate. At present, the more commonly used linking agent is adipic hydrazide. The -NH2 at both ends can react and bond with the cyanate ester group on the polysaccharide and the carboxyl group of the carrier protein respectively in the presence of carbodiimide.
Other Methods
The covalent combination of polysaccharides and carrier proteins can be coupled with different linkers based on different functional groups. The available functional groups on the surface of polysaccharides mainly include -OH, -COOH and -NH2, and the available groups on the surface of carrier proteins mainly include -COOH, -NH2, -SH, and OH.
Factors Affecting the Immunogenicity of Pneumonia Conjugate Vaccine
Carrier Protein
Carrier protein is one of the important factors affecting the immunogenicity of pneumonia conjugate vaccine. Any protein carrying T cell helper epitopes can be used as a carrier protein for conjugated vaccines. Vaccine manufacturers often use proteins with good safety, easy production, low cost and high yield.
Sugar Chain Length
The oligosaccharide pool used in the preparation of Streptococcus pneumoniae polysaccharide conjugates generally consists of polysaccharides or oligosaccharide fragments obtained through degradation. The length of the sugar chain (oligosaccharide or polysaccharide) of these “sugar fragments” is uncertain and uneven. Different sugar chain lengths may have a greater impact on the immunogenicity of conjugate vaccines.
Combination
The binding methods between polysaccharides and proteins are mainly divided into direct binding and indirect binding. Direct binding utilizes polysaccharides and proteins.
The functional groups on the surface perform organic bonding; indirect binding uses “bridging agents” to link polysaccharides and proteins. The two combination methods may have an impact on the immunogenicity of the pneumonia conjugate vaccine. This is mainly reflected in the fact that the bridging linker has both a “bridge” function and may also reduce the shielding effect (the spatial shielding of polysaccharide epitopes by bulky proteins). function, and the nature of the linker may also affect the expression of immunogenicity of the pneumonia conjugate vaccine.
Other Factors
Studies have shown that adding high doses of free sugars to the Streptococcus pneumoniae type 4 polysaccharide protein conjugate vaccine reduces the immunogenicity of the conjugate.