In 1924, the German physiologist Otto Warburg found that the growth of cancer cells was heavily dependent on glycolysis compared to normal cells, and this process produced a large amount of “metabolized waste” lactic acid, which is known as the “Waborg effect.” Compared to other metabolic pathways, glycolysis that produces lactic acid is not advantageous for high energy consumption cancer cells, and the abnormal behavior of high energy consumption cancer cells choosing glycolysis as the main pathway of energy has plagued scientists for decades.
Of course, the tumor favors the glycolysis of lactic acid production, certainly not for a yoghurt, but to make it more suitable for its growing environment. It is well known that most tumor cells are in a low-oxygen environment, so the oxygen-free glycolysis pathway is chosen for energy supply. But is it only for this reason?
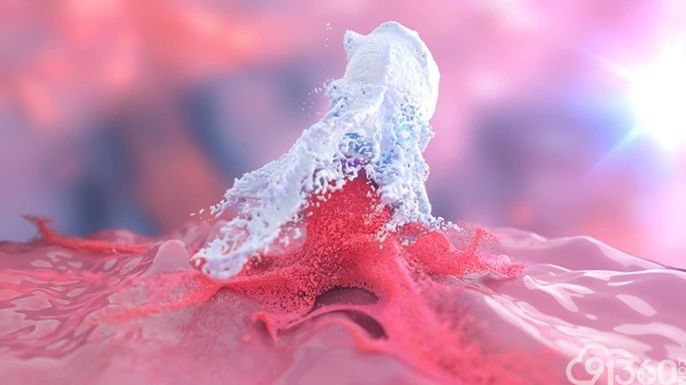
Recently, scientists from the University of Chicago team Professor Zhao Yingming and scientists at the Rockefeller University have finally unveiled this mystery. They found that lactic acid is not only a metabolite of glycolysis, it can also be linked to the histones of the macrophage genome by epigenetic modifications, regulating the switching of related genes. And more importantly, it is also first discovered that lactic acid can be used as an epigenetic modification after histone translation to regulate gene expression. This breakthrough discovery gives us a new understanding of the function of lactic acid and will prompt scientists to re-examine the “Waberg effect.”
Lactic acid is known to be the end product of the “Wabberg effect,” but it has been treated as a metabolic waste for a long time. In recent years, some scientists have discovered that lactic acid can be perceived by some immune cells, which in turn creates an immunosuppressive environment for tumors. It has also been found that lactic acid can be converted to acetic acid by tumor-associated fibroblasts for use by cancer cells.
Mechanism of Lactic Acid Regulation Related Genes
In order to further unravel the mechanism of lactate regulation genes, the researchers conducted further exploration. Based on previous studies on the modification of histones by cellular metabolites, they speculated that the lactation acid of histones might occur on the amino acid lysine. Through mass spectrometry, as well as techniques such as isotope tracing and immunoblotting, they finally determined that the lactation modification of histone lysine is indeed widespread in human and mouse cells. Subsequent cell experiments have also shown that the lactation of histones is regulated by glycolysis. Moreover, the lactic acidation of lysine on histones is highly sensitive to lactic acid produced by glycolysis, and varies with the strength of glycolysis or the level of lactic acid.
So What Is the Function of Histone Lactation?
The researchers studied this problem using macrophages as a model. They found that if pro-inflammatory M1 macrophages produce large amounts of lactic acid, the histone lactic acid level of the promoter region of some genes will increase, the gene will be opened, the expression level will increase, and the M1 type macrophages will be transformed into M2 type.
In fact, under normal circumstances, this is a protection mechanism. Macrophages encounter bacterial infections and, under the stimulation of bacterial lipopolysaccharide, become M1 macrophages, promote inflammation and eliminate pathogens. At the same time, macrophages also initiate glycolysis and produce lactic acid. As the level of lactic acid accumulates, the level of histone lactate increases, and macrophages are transformed into anti-inflammatory M2, avoiding some damages of body. However, this mechanism is just used by tumor cells to promote tumor growth, metastasis and immunosuppression.
In general, this study reveals an unknown aspect of lactic acid. Lactic acid and lactation, which link human metabolism to gene expression, may have found a new key point for scientists to study disease.
