Respiratory tract infection is an important cause of human morbidity and death worldwide and one of the main causes of death in children under 5 years old. Since 2001, researchers in the Netherlands reported a new virus related to respiratory tract infections in humans, especially infants – human metapneumovirus (HMPV), and the virus has been detected successively in the United States, Canada, Europe and other countries. This article reviews the virological, epidemiological, and clinical features of HMPV.
Virological characteristics of HMPV
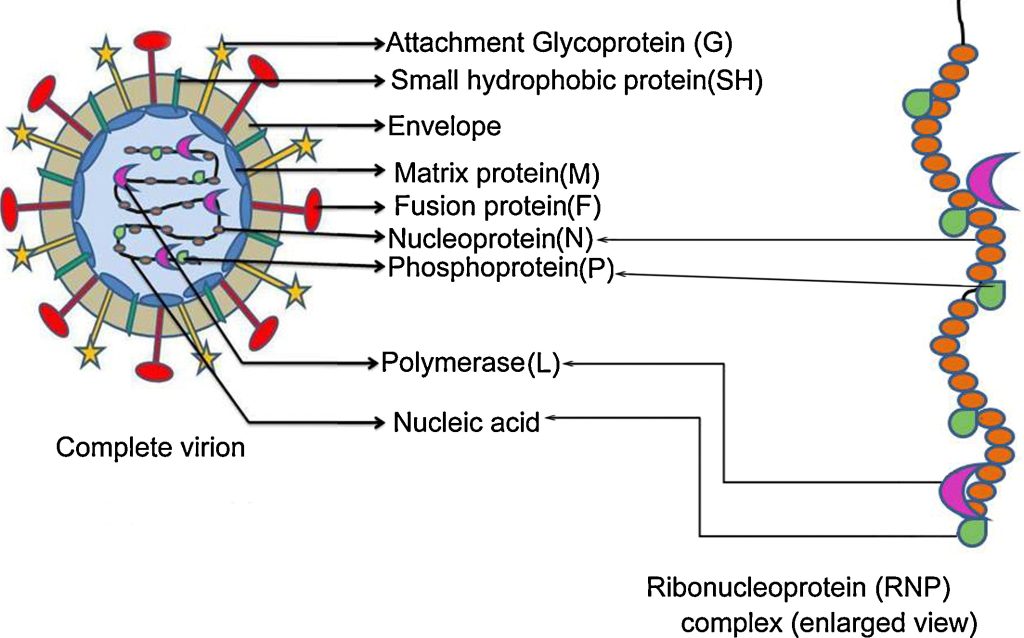
Figure 1. Schematic diagram of the human metapneumovirus particle and the ribonucleoprotein (RNP) complex.
The morphology of HMPV virus particles is consistent with that of the genus Paramyxovirus, and it belongs to the subfamily Pneumoviridae of the family Paramyxoviridae. It is similar to avian metapneumovirus (APV). Sequence analysis showed that the amino acid homology between HMPV and APV-C was as high as 80%. Although HMPV is closely related to APV-C, their host ranges are different, which may be related to the difference of SH and G proteins of the two viruses. The total length of the HMPV genome is about 13kb. It is a single-stranded negative-sense RNA containing 8 genes and 9 open reading frames corresponding to the gene arrangement, and the 5′ encodes 9 different proteins. Contains encoding nucleoprotein (N), phosphoprotein (P), matrix protein (M), fusion gene (F), transcription elongation factor/RNA synthesis regulator (M2), small hydrophobic (SH) surface protein, major invasion (G ) glycoprotein, polypolymerase (L) subunit and other genes. Among them, F, G and SH are transmembrane surface proteins, and N, P and L together form the nucleocapsid protein. According to the difference of F, G, and P gene sequences, HMPV can be divided into two types, A and B, and at least four subtypes (A1, A2, B1, B2). Two genotypes of HMPV can circulate in the same year. According to the laboratory research of Biacchesi et al., it is found that the nucleotide and amino acid homology levels of A and B genotypes are as high as 80% and 90%, respectively. The main difference between the subtypes is in the SH and G genes. Many scholars believe that it is because of the differences and great homology between different genotypes that the same patient can have multiple HMPV infections at different times, and at the same time, the body can not fully immunity respond to HMPV infections at different times. As for whether their antigen types are different due to differences in genotypes, further research on antibodies in serum is required.
Epidemiological Characteristics of HMPV infection
Seasonal distribution
According to the current research, the infection caused by HMPV mainly occurs in winter, especially from December to January of the following year, which is the peak period of virus prevalence and detection. From November 2001 to October 2002, Esper of Yale University in the United States collected the respiratory secretions of 794 patients with respiratory tract infection for virus isolation and identification, and obtained respiratory syncytial virus (RSV), HMPV, influenza virus (A, B) and Parainfluenza virus. Among them, HMPV infection is mainly seen from December to April of the next year, which is similar to the distribution of RSV. Therefore, the possibility of virus infection should be considered when respiratory symptoms appear in winter and spring. HMPV was rarely detected and isolated in summer. However, due to the lack of current data, especially the lack of data on HMPV infection in summer, no conclusions can be drawn on the prevalence of HMPV in summer.
Age Distribution
Since vanden Hoogen et al. first isolated HMPV from children with acute respiratory infection, most of the studies were aimed at children. Most people think that HMPV mainly infects children, and the infection rate of infants aged 0-1 years is the highest, and most HMPV infections occur in the first year of life; however, later studies found that HMPV infection is related to severe acute respiratory tract infection in the elderly or immunocompromised, and it is also the pathogen of human community-acquired acute respiratory tract infection. According to current research, HMPV can infect infants from 2 months to 99-year-olds, indicating that people may be infected throughout their lives. Susceptible objects are infants and immunocompromised adults and the elderly, but the infection among young people Most common.
Population Infection Rate
In a study in the Netherlands, all children under 6 years of age were serologically positive, suggesting that most children had been infected with the virus. Some scholars have detected HMPV in 7% of patients with acute respiratory infection in hospitals. Canadian researchers found that the HMPV infection rates of <5 years and >65 years were 35.1% and 45.9%, respectively. 17% of children with lower respiratory tract infection in the study by Cuevas et al. were HMPV infected; Vicente et al. found that 4.1% of children with community-acquired acute respiratory tract infection were infected with HMPV.
Clinical Features of HMPV Infection
HMPV appears to have a tropism for the respiratory epithelium and can cause acute respiratory infections in children. HMPV infection in children can range from mild respiratory illness to severe cough, bronchitis, pneumonia usually accompanied by high fever, myalgias and vomiting. Patients should be treated and require ventilator-assisted breathing. The main symptoms are cough, rhinitis, fever, dyspnea, wheezing, difficulty eating, hyperventilation, tachycardia, cyanosis, etc.; the clinical symptoms of adult infection are not obvious, mainly including nasal congestion, dyspnea, wheezing, coughing, etc., but fever is rare; in the elderly, dyspnea and wheezing are more common than in the young and middle-aged, and the hoarseness of the young and middle-aged is more than the elderly. HMPV is either independent or coexists with RSV and shares a common seasonal distribution with RSV. The clinical manifestations of HMPV infection are not characteristic, and are similar to other respiratory virus infections such as RSV and Inf.